twosmek
Guest
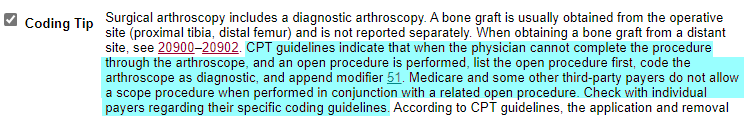
The md started out with doing the procedure arthroscopically and then had to open the incision. The applicable documentation is as follows. (He did scope other compartments for the knee prior to this)--Preforming MD wanted to code 27599 (unlisted), I was thinking 27514, or 29885 with a 22 modifier.
Please help @!>?%#
Postoperative DX; Chondral delaminated flap flexion surface of the lateral femoral condyle (18x15mm)
Procedure: Internal fixation of full thikness articular cartilage delamination lateral femoral condyle with Arthrex bioabsorbable compression screws.
The loose delaminating posterior flap of articular cartilage was felt to be unstable in the patient's young age and the large amount of weightbearing surface involved, it was felt indicated proceed with fixation of that fragment of cartilage. This was done with an Arthrex 2 mm compression screw. This was advanced initially arthroscopically. As the screw was fully seated there was a suprising amount of purchase obtained which did not allow full seating of the screw before the head stripped down. The remaining prominent 2 mm of the implant was then difficult to access arthroscopically. The lateral portal was therefore extended into a short lateral retinacular incision to visually expose the delamination site. The prominent end of the implant was trimmed back with the rongeur and then smoothed with an arthroscopic burr to be flush below the articular surface. This was noted to nicely secure the posterior most portion of the flap, hoever, the anterior leading edge was still somewhat unstable and then that was secured with a second screw placed in standard fashion, again despite drilling for 28 mm implant and selecting 24, the compression achieved stell exceeded tolerance of the insertion driver and was left somewhat prominent before stripping off the head, therefore, that was then also planed flush with teh articular surface. Probing the leading margin of the articular flap then proved stable. The wound was irrigated. A lateral retnacular split was closed with interrupted o vicry, buried 2-0 Monocryl was used subcutaneously followed by interrupted nylon suture for skin.
Please help @!>?%#
Postoperative DX; Chondral delaminated flap flexion surface of the lateral femoral condyle (18x15mm)
Procedure: Internal fixation of full thikness articular cartilage delamination lateral femoral condyle with Arthrex bioabsorbable compression screws.
The loose delaminating posterior flap of articular cartilage was felt to be unstable in the patient's young age and the large amount of weightbearing surface involved, it was felt indicated proceed with fixation of that fragment of cartilage. This was done with an Arthrex 2 mm compression screw. This was advanced initially arthroscopically. As the screw was fully seated there was a suprising amount of purchase obtained which did not allow full seating of the screw before the head stripped down. The remaining prominent 2 mm of the implant was then difficult to access arthroscopically. The lateral portal was therefore extended into a short lateral retinacular incision to visually expose the delamination site. The prominent end of the implant was trimmed back with the rongeur and then smoothed with an arthroscopic burr to be flush below the articular surface. This was noted to nicely secure the posterior most portion of the flap, hoever, the anterior leading edge was still somewhat unstable and then that was secured with a second screw placed in standard fashion, again despite drilling for 28 mm implant and selecting 24, the compression achieved stell exceeded tolerance of the insertion driver and was left somewhat prominent before stripping off the head, therefore, that was then also planed flush with teh articular surface. Probing the leading margin of the articular flap then proved stable. The wound was irrigated. A lateral retnacular split was closed with interrupted o vicry, buried 2-0 Monocryl was used subcutaneously followed by interrupted nylon suture for skin.