- Messages
- 8
- Best answers
- 0
Good morning,
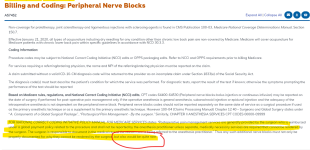
We have recently started billing for our own anesthesia services. It looks like Medicare is separating the claim, and rejecting the postop pain blocks.
We are utilizing the 59 modifier, the anatomic modifier for side (LT or RT) and are writing a description of the block, specifying that it is requested by the surgeon for postop pain.
These are the denial descriptors:
MA15 Alert: Your claim has been separated to expedite handling. You will receive a separate notice for the other services reported.
N211 Alert: You may not appeal this decisionM52 Missing/incomplete/invalid “from” date(s) of service.
N345 Date range not valid with units submitted.
Does anyone have any insite into this?
Thanks!
We have recently started billing for our own anesthesia services. It looks like Medicare is separating the claim, and rejecting the postop pain blocks.
We are utilizing the 59 modifier, the anatomic modifier for side (LT or RT) and are writing a description of the block, specifying that it is requested by the surgeon for postop pain.
These are the denial descriptors:
MA15 Alert: Your claim has been separated to expedite handling. You will receive a separate notice for the other services reported.
N211 Alert: You may not appeal this decisionM52 Missing/incomplete/invalid “from” date(s) of service.
N345 Date range not valid with units submitted.
Does anyone have any insite into this?
Thanks!