Brenda1973
Networker
- Messages
- 94
- Best answers
- 0
Outpatient coding question here: Known fact that terminology such as , "suspected, possibly, probable, likely, consistent with, ect. " are all terms that according to guidelines cannot be documented for a diagnosis in the assessment and used for a definitive diagnosis. I understand they cannot be documented in the assessment, but my question is can that verbiage be documented in the plan? Verbiage is bolded in 2 examples below: 1st example Plan states, "suspected strep" and second example plan states "possible allergic reaction." Can someone tell me if this is acceptable verbiage to be documented in the plan and used for a diagnosis as well. Thank you.
Assessment
- Streptococcal pharyngitis
Plan
- Prescribed amoxicillin and sent the prescription to the patient's pharmacy for treatment of suspected streptococcal pharyngitis.
- Advised to discard the current toothbrush and replace it with a new one approximately 3 to 4 days after starting the antibiotic course to reduce the risk of reinfection.
Centor criteria score: 3 with close contact
Diagnosis Plan
1. Acute streptococcal pharyngitis amoxicillin (Amoxil) 500 mg capsule
------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
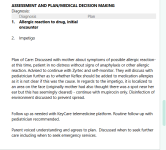
ASSESSMENT AND PLAN/MEDICAL DECISION MAKING
Diagnosis:
Diagnosis Plan
1. Allergic reaction to drug, initial encounter
2. Impetigo
Plan of Care: Discussed with mother about symptoms of possible allergic reaction- at this time, patient in no distress without signs of anaphylaxis or other allergic reaction. Advised to continue with Zyrtec and self-monitor. They will discuss with pediatrician further as to whether Keflex should be added to medication allergies as it is not clear if this was the cause. In regards to the impetigo, it is localized to an area on the face (originally mother had also thought there was a spot near her ear but this has seemingly cleared) - continue with mupirocin only. Disinfection of environment discussed to prevent spread.
Assessment
- Streptococcal pharyngitis
Plan
- Prescribed amoxicillin and sent the prescription to the patient's pharmacy for treatment of suspected streptococcal pharyngitis.
- Advised to discard the current toothbrush and replace it with a new one approximately 3 to 4 days after starting the antibiotic course to reduce the risk of reinfection.
Centor criteria score: 3 with close contact
Diagnosis Plan
1. Acute streptococcal pharyngitis amoxicillin (Amoxil) 500 mg capsule
------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
ASSESSMENT AND PLAN/MEDICAL DECISION MAKING
Diagnosis:
Diagnosis Plan
1. Allergic reaction to drug, initial encounter
2. Impetigo
Plan of Care: Discussed with mother about symptoms of possible allergic reaction- at this time, patient in no distress without signs of anaphylaxis or other allergic reaction. Advised to continue with Zyrtec and self-monitor. They will discuss with pediatrician further as to whether Keflex should be added to medication allergies as it is not clear if this was the cause. In regards to the impetigo, it is localized to an area on the face (originally mother had also thought there was a spot near her ear but this has seemingly cleared) - continue with mupirocin only. Disinfection of environment discussed to prevent spread.