Bust 4 Common Holter Monitor Coding Myths to Submit Clean Claims
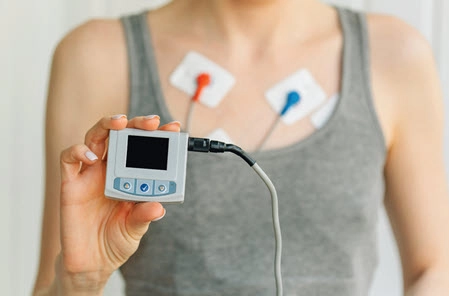
Educate your physicians about documentation guidelines. If your cardiologist performs Holter monitoring, you know this can be a challenging service to report. Not only do you have to understand the rules regarding third-party Holter equipment owners, but you must also know the exact length of the analysis time. Shatter the following myths to keep your Holter monitor coding running smoothly. Myth 1: You Don’t Have a Global Code Choice for Holter Monitoring Reality: Code 93224 (External electrocardiographic recording up to 48 hours by continuous rhythm recording and storage; includes recording, scanning analysis with report, review and interpretation by a physician or other qualified health care professional) is the global code for Holter monitoring. Code 93244 is only billable by the physician when they are providing all of the components of a 24-48-hour Holter service, which includes the recording, scanning analysis with the report (this is not the physician’s report; it is the report of the actual analysis itself), and the review and interpretation (which is the physician’s report), says Mari Robinson, CPC, CCC, CRC, CPMA, compliance analyst of chronic conditions at Riverside Medical Group in Newport News, Virginia. Don’t miss: The physician must own the Holter equipment to bill code 93224, according to Robinson. “It has become so expensive for physicians to own their own equipment for this that most times the equipment is supplied by an outside source,” she says. In that case, you wouldn’t report 93224. Read on for your other coding options. Myth 2: Billing Rules Don’t Change When Third Party Supplies Holter Equipment Reality: When a third party supplies the physician with the Holter equipment, the global code is then broken apart and submitted with the individual codes for each component being billed, rather than 93244, according to Robinson. The billing for physician or professional services would normally occur as follows, per Robinson: Myth 3: Analysis Time Isn’t Vital Reality: As a coder, an important part of billing for a Holter monitor is reviewing the report for the analysis time that actually occurred, Robinson says. You should carefully review and read the report to identify the analysis time and the type of monitor you are billing for, she adds. “Within the top patient area of the report, you will find the patient’s name, date of birth, and demographic information, including the diagnosis you will need to report the hook-up billing,” according to Robinson. “Somewhere within that information at the top of the report, you will see the ‘analysis time.’ It will include the start date and end of service date you will need to verify if it is an actual Holter monitor.” If the analysis time is longer than 48 hours, you should not report 93244, 93225, or 93227. Holter monitoring is used when the provider wants to monitor the patient for up to 48 hours, explains Ray Cathey, PA, FAAPA, MHS, MHA, CCS-P, CMSCS, CHCI, CHCC, president of Medical Management Dimensions in Stockton. Monitoring for more than 48 hours would require documentation of medical necessity and justification that codes 93241 (External electrocardiographic recording for more than 48 hours up to 7 days by continuous rhythm recording and storage; includes recording, scanning analysis with report, review and interpretation)-93248 (External electrocardiographic recording for more than 7 days up to 15 days by continuous rhythm recording and storage …) would be more appropriate. Be sure to review the documentation to verify what type of monitor was used for the patient, adds Robin Peterson, CPC, CPMA, manager of professional coding services, Pinnacle Integrated Coding Solutions, LLC in Centennial, Colorado. “Most third-party monitor companies will supply the physician’s office with a weekly and monthly spreadsheet of all the monitors they have billed with the 93226 technical code,” she adds. “This will help you determine which monitor code to use as well, but confirmation is always the analysis time reported on the actual report.” Myth 4: There Aren’t Any Challenges With Holter Monitoring Reality: Coders will encounter several challenges when reporting and billing for Holter monitors. “There are different types of monitors, so it is extremely important to bill for the correct monitor,” Robinson says. “They each have their own code set: Holter monitors, event monitors, and cardiac telemetry monitors.” When it comes to third-party monitor companies, they will help the physician’s office or coder with monitor billing, according to Robinson. “They have a department specifically designed to help with payer issues, and it is very valuable. Take advantage of that,” she says. “The monitor rep will help you with payer issues if you contact them and tell them you are having reimbursement problems.” Robinson adds that it is valuable to ask the monitor rep to do an “in-service” in your office for all of your clinical and coding staff. “This will help each person understand the different types of monitors and how they work,” she says. “Many monitors are automatic and also patient-activated.” As a coder, the reps will help you understand how they preauthorize the monitor and how a monitor can “move into another monitoring” device, as well, as if that new level of monitor will be reimbursed by the payer, Robinson says. Finally, communicate with your physicians, Robinson says. “Establish a rapport with the physician, if you can, to help them understand the documentation guidelines and requirements for specific monitors such as MCots (MCT) and loop recorder implants,” she says. “These monitors have a more specific and defined report and require a different level of documentation from the physician or provider in order to establish the proper criteria and medical necessity to be able to use these monitors.”