Can You Answer These Inpatient E/M Coding FAQs?
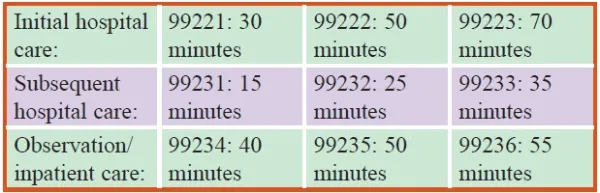
Hint: Don’t forget modifier AI when necessary. Whether your ob-gyn is seeing hospital patients following trauma, infections, balance issues, or after surgery, you absolutely must know how to report the inpatient evaluation and management (E/M) codes. But although the outpatient coding rules changed in 2021, you’ll still need to use the 1995 or 1997 guidelines for history, exam, and medical decision making (MDM) components to report these services accurately. Check out a few of the most frequent inpatient coding questions submitted to Ob-Gyn Coding Alert, along with the solutions that will help you report these services accurately in the future. Question 1: How Should I Code for an Admission? Answer: Although coders commonly pore over the CPT® code book looking for an admission code, you should save the time before you go on the hunt. That’s because there aren’t any codes that relate specifically to hospital admissions. Instead, you’ll report one of the following codes for initial inpatient services for the admitting physician: The tricky part is knowing which provider is considered the “admitting physician.” That’s because only one physician admits the patient to the hospital. Anyone else billing initial hospital care is seeing the patient as a replacement for the consultation codes, and CMS has instructed consulting physicians to code initial hospital care even when they are not the admitting physician. One easy way to break it down is to remember that for Medicare, the admitting service is identified with modifier AI (Principal physician of record). All other providers should bill the inpatient E/M codes that describe their participation in the patient’s care (i.e., subsequent hospital visit, or inpatient consultation [99251- 99255]). In the case of Medicare, consultants will not be able to report 99251-99255 — instead, they are required to use 99221-99223, because Medicare no longer pays for consultations. Regardless of the service type, only one claim can be reported per patient per specialty per patient per day. For example, if ob-gyn Jones sees the patient in the morning and ob-gyn Smith, who is covering for Jones, sees the same patient in the evening, the notes for both services are combined and only one hospital visit is coded. However, if two physicians see the patient and they are in different specialties and are seeing the patient for different reasons, then both may bill a hospital visit based on that physician’s note and the medical necessity of the service. Question 2: When Should I Use 99234-99236 for Initial Inpatient Care? Answer 2: In some cases, your ob-gyn may see a patient who has been admitted to observation care, or who is admitted and discharged to observation on the same date. In these instances, you may look toward this code range: The basic difference between the 99221-99223 range and these codes is that 99234-99236 represents the services of an initial hospital observation service and a discharge service performed on the same calendar date. This means your documentation must reflect the exact times for admission and discharge. To bill 99234-99236, you must have a statement that shows the stay for observation care was greater than eight hours but less than 24 hours. If the admission lasts more than 24 hours, then you may consider using 99221-99223 for the initial day of hospital care. However, there are instances where a patient can be in observation for up to 48 hours, in which case you’ll report code range 99218-99220 (Initial observation care…) alongside 99217 (Observation care discharge day management…) on the discharge date. It’s important to note that a patient can be in an inpatient bed, but still be considered in observation as an outpatient in some instances. Question 3: How Should I Document Hospital Care? Answer 3: First, the initial inpatient codes require you to document that the three key components of history, examination, and MDM appropriate to their levels have been met. The level of the encounter will be determined by the lowest documented level of the history, exam, and MDM since all three must be met for these codes. Weak documentation in one will pull the encounter down. Both the level 2 and 3 initial hospital visits require a comprehensive history and exam. The only difference is the MDM, with the level 2 requiring moderate and the level 3 requiring high. So, if the documentation of the history or exam do not reach a comprehensive level, the initial hospital service is held down to a level 1 or may not even meet the requirements for the first level. Additionally, because 99234-99236 represent both observation and hospital services, the documentation should support both services. Question 4: Can You Code Inpatient Visits Based on Time? Answer 4: Yes, you are able to code your inpatient visits based on time if counseling and coordinating care represents over 50 percent of the encounter time. But this can lead to some problems when determining which codes you should be reporting. Time is often underdocumented for inpatient E/M services. Providers don’t always remember to document time that is spent on the unit/floor that is outside the face-to-face time with the patient and family. Inpatient E/M time-based claims also require that more than 50 percent of the total visit time is spent counseling or coordinating care. Another important thing to remember is the typical time for each code is different, as the following chart shows: Question 5: How Should I Report Hospital Discharges? Answer 5: When the provider discharges the patient, you’ll choose from one of the following codes, depending on the encounter specifics: Important: Keep in mind that the discharge service is bundled into most procedure codes and would therefore generally not be reportable if a procedure was performed by the discharging physician during the hospitalization. When you can rightfully report 99238 or 99239, the codes include the following services in their work units: The documentation should include the final exam elements as well as the information around the discharge — i.e., education, meds, follow-up, course of care, etc. — along with the time spent in the activity of the discharge. If no time is documented, it is assumed that 30 minutes or less was spent on discharge services and only a 99238 may be coded. Source: Palmetto GBA Comparative Billing Report for E/M Services.