pclaybaugh
Guru
Looking for feedback from others coding orthopaedics: my group is adding E/Ms to most 20610 joint injections—even when the entire visit focuses on that joint alone.
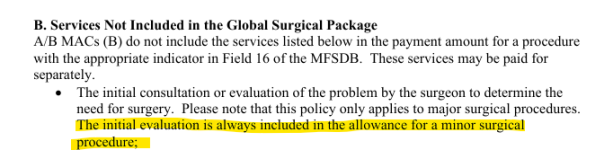
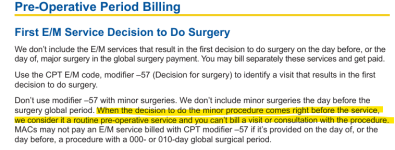
Per the 2025 NCCI Manual, Ch. IV, p. 4, the eval is included in the procedure. An E/M should only be billed if there’s a separate diagnosis and management unrelated to the injected joint.
Here’s a sample note—they’re calling this a new issue, but I don’t think it justifies an E/M:
Chief Complaint
Left knee pain. X-rays taken today. History of Present Illness
Patient presents today for a new issue. He is here today for his left knee. He reports a traumatic history involving the left lower extremity. He has had multiple surgeries with fixation of his femur and his tibia. He has had an onset of pain in the left knee and felt like he noted some swelling. The pain has improved but is still bothering him. He is here for evaluation of this today.
Physical Exam Vitals & Measurements
ROS: Alert and oriented, well nourished, No acute distress
Lungs: Respiration: Non-Labored
Abdomen: Soft, non-tender, non-distended, Normal bowel sounds, No masses
Musculoskeletal: Left knee: Noted varus alignment. Skin is intact with well-healed scars about the anterior lateral aspect of the distal thigh and proximal tibia. Range of motion 0-15 degrees. Stable varus/valgus stress. Mild tenderness palpation at the medial joint line.
Skin: Skin is warm, dry and pink, No rashes, No lesions
Psychiatric: Cooperative, appropriate mood and affect Procedure Injection left knee
After obtaining informed consent, the left knee is prepped and draped in usual sterile fashion. Through an anterolateral approach the left knee is injected with an admixture of 1 cc of 40 mg Kenalog 2 cc of 1% lidocaine without epinephrine. Patient tolerated the injection well a sterile Band-Aid is applied. Instructed in postinjection care.
Assessment/Plan
Left knee posttraumatic osteoarthritis
He has had terrible trauma to the left lower extremity that was fixed appropriately. Unfortunately appears he has gone on to posttraumatic osteoarthritis. We have discussed this in depth. Further surgical intervention would only be conversion to a total knee arthroplasty. He is not at a point where he is interested in pursuing this. We have also talked about management with corticosteroid injection. He would like to try an injection to the left knee today. We will inject the left knee and I will see him back in 3 months for reevaluation.
Medications and Immunizations This Visit Given Kenalog-40, 40 mg, 2 mL, Intra-articular. For: Osteoarthritis of left knee
Anyone else had to push back on this? Would appreciate your take.
Many thanks!!
Per the 2025 NCCI Manual, Ch. IV, p. 4, the eval is included in the procedure. An E/M should only be billed if there’s a separate diagnosis and management unrelated to the injected joint.
Here’s a sample note—they’re calling this a new issue, but I don’t think it justifies an E/M:
Chief Complaint
Left knee pain. X-rays taken today. History of Present Illness
Patient presents today for a new issue. He is here today for his left knee. He reports a traumatic history involving the left lower extremity. He has had multiple surgeries with fixation of his femur and his tibia. He has had an onset of pain in the left knee and felt like he noted some swelling. The pain has improved but is still bothering him. He is here for evaluation of this today.
Physical Exam Vitals & Measurements
ROS: Alert and oriented, well nourished, No acute distress
Lungs: Respiration: Non-Labored
Abdomen: Soft, non-tender, non-distended, Normal bowel sounds, No masses
Musculoskeletal: Left knee: Noted varus alignment. Skin is intact with well-healed scars about the anterior lateral aspect of the distal thigh and proximal tibia. Range of motion 0-15 degrees. Stable varus/valgus stress. Mild tenderness palpation at the medial joint line.
Skin: Skin is warm, dry and pink, No rashes, No lesions
Psychiatric: Cooperative, appropriate mood and affect Procedure Injection left knee
After obtaining informed consent, the left knee is prepped and draped in usual sterile fashion. Through an anterolateral approach the left knee is injected with an admixture of 1 cc of 40 mg Kenalog 2 cc of 1% lidocaine without epinephrine. Patient tolerated the injection well a sterile Band-Aid is applied. Instructed in postinjection care.
Assessment/Plan
Left knee posttraumatic osteoarthritis
He has had terrible trauma to the left lower extremity that was fixed appropriately. Unfortunately appears he has gone on to posttraumatic osteoarthritis. We have discussed this in depth. Further surgical intervention would only be conversion to a total knee arthroplasty. He is not at a point where he is interested in pursuing this. We have also talked about management with corticosteroid injection. He would like to try an injection to the left knee today. We will inject the left knee and I will see him back in 3 months for reevaluation.
Medications and Immunizations This Visit Given Kenalog-40, 40 mg, 2 mL, Intra-articular. For: Osteoarthritis of left knee
Anyone else had to push back on this? Would appreciate your take.
Many thanks!!