Hello,
I am currently training my Urology doctors on the new E/M changes for 2021. Can someone tell me what they are saying to their doctors regarding Cat 2 "Amount and/or Complexity of Data to be Reviewed and Analyzed?
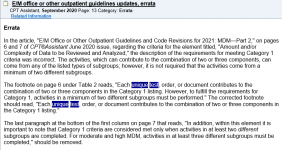
My question is related to the ordering of unique tests. In order to bill for a moderate level (99214 or 99204) the chart below states that they can order and review a unique test (lab) and receive credit for both.
An example, doctors order a UA lab test and review on the same day, that would give them 2 points one for the order and one for the review?
Also, do they only need to meet one of the 3 categories to meet the data required for Moderate? I am not sure if I am interpreting this correctly and my doctors are in disbelief that it will be this easy to bill for a moderate level.
Moderate 99214 of 99204
(Must meet the requirements of at least 1 out of 3 categories)"
Category 1: Tests, documents, or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source*;
• Review of the result(s) of each unique test*;
• Ordering of each unique test*;
• Assessment requiring an independent historian(s) or
Category 2: Independent interpretation of tests
"• Independent interpretation of a test performed by another physician/other qualified health care
professional (not separately reported); or"
Category 3: Discussion of management or test interpretation (Discussion of management or test interpretation with external physician/other qualified health care professional\appropriate source (not separately reported)
I am currently training my Urology doctors on the new E/M changes for 2021. Can someone tell me what they are saying to their doctors regarding Cat 2 "Amount and/or Complexity of Data to be Reviewed and Analyzed?
My question is related to the ordering of unique tests. In order to bill for a moderate level (99214 or 99204) the chart below states that they can order and review a unique test (lab) and receive credit for both.
An example, doctors order a UA lab test and review on the same day, that would give them 2 points one for the order and one for the review?
Also, do they only need to meet one of the 3 categories to meet the data required for Moderate? I am not sure if I am interpreting this correctly and my doctors are in disbelief that it will be this easy to bill for a moderate level.
Moderate 99214 of 99204
(Must meet the requirements of at least 1 out of 3 categories)"
Category 1: Tests, documents, or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source*;
• Review of the result(s) of each unique test*;
• Ordering of each unique test*;
• Assessment requiring an independent historian(s) or
Category 2: Independent interpretation of tests
"• Independent interpretation of a test performed by another physician/other qualified health care
professional (not separately reported); or"
Category 3: Discussion of management or test interpretation (Discussion of management or test interpretation with external physician/other qualified health care professional\appropriate source (not separately reported)