CXZook
Contributor
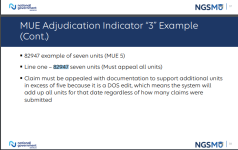
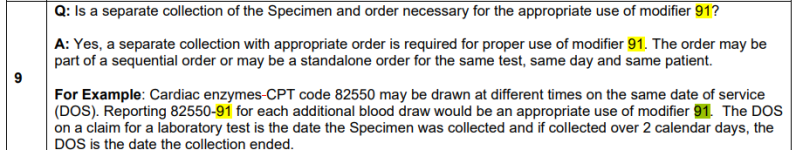
Patient has a total of 8 glucose test repeated on the same date of service. We are billing CPT 82947. Would modifier 91 be added to every 82947 except the 1st 82947 charged? Or does 91 get added the charges that exceed MUE? MUE is 5 so the 6th, 7th, and 8th 82947 that is charged.