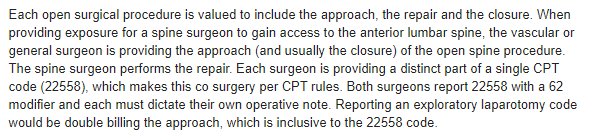
We are having an internal debate on what the appropriate codes would be for a cardiovascular surgeon assisting with a spinal fusion. Would the correct code for the procedure below be 37617? The other provider completed the actual instrumentation.
PREOPERATIVE DIAGNOSIS:
Lumbosacral disk disease.
POSTOPERATIVE DIAGNOSIS:
Lumbosacral disk disease.
OPERATIVE PROCEDURE:
Anterior exposure for L4-L5 anterior lumbar interbody fusion with placement of cage and screws .
INDICATION:
This is a pleasant 60-year-old with severe lumbosacral disc disease and spondylolisthesis being scheduled for anterior lumbar interbody fusion, posterior instrumentation. The patient had a previous fusion at L5-Sl. She is now being taken to the operating room for her unstable L4-L5. The patient is aware of options and risks.
DESCRIPTION OF OPERATIVE PROCDURE
The patient was placed on her back on the operating table. General endotracheal anesthesia was administered without difficulty. Foley catheter and radial art line were placed. The abdomen was shaved, prepped and draped in the usual sterile fashion. After a brief preoperative time-out, the patient had an 8 em left paramedian incision made beginning just to the left of the umbilicus and extending down. It was carried down through subcutaneous tissue with Bovie electrocautery. The fascia was divided along the lines of skin incision. Medial aspect of the fascia was grasped with 2 Kelly clamps. The rectus was gently teased away from the posterior rectus sheath and retracted towards the left. Sponge s tick was used to help elevate the inferior epigastric artery and vein. The retroperitoneum was entered. A small portion of lateral flexion of posterior rectus sheath was divided with Bovie electrocautery and extended tip. Peritoneal contents were retracted towards the right. Psoas was visualized and genitofemoral nerve was avoided. Bookwalter retractor was set up with the post on the right using a small ring. Three blades were positioned. Dissection was carried out just to left of the left iliac artery. Bipolar electrocautery was necessary to divide some of the very small lymphatics to retract them to the left. Dissection was carried down on to a large segmental vein, right at the top of L4. This was ligated with 2-0 silk suture ligated with 5-0 Prolene, clipped and divided. The iliolumbar vein below the L4-L5 level was then identified. It was ligated with 2-0 s ilk suture ligated with 5-0 Prolene, clipped and divided. At that point, we just dissected the vessel off of the anterior surface of that ligament over L4-L5. There were several small venous perforators, which were coagulated with bipolar electrocautery and divided. The vein was mobilized without too much trouble and a bent spinal needle was then placed in the disk space. We confirmed that we are in the midline and at the appropriate level. I marked the midline with Bovie electrocautery and renewed the needle. At that point, Dr. _______ came into the room. He did his diskectomy at L4-L5 and placed a cage with 2 screws for fixation. A small amount of FloSeal was placed for complete hemostasis. The retractor blades were reviewed. Sponge, instrument and needle counts were correct. Final films were done, 4-quadrant films were done. The ureter, iliac artery and vein and inferior epigastric artery and vein were all seen to be without any injury. Pulse ox in left great toe read 1 000/o sat. The pulse in left foot was normal. SSEPs were baseline. The fascia of the rectus was closed with #1 Vicryl, one beginning superiorly and one inferiorly, tied in middle. Subcutaneous tissue was closed with two layers of 2-0 Vicryl and the skin with 3-0 Monocryl in a subcuticular fashion. Steri-Strips and dry sterile dressings were applied. The patient was then returned to the prone position for further instrumentation, dictated under separate cover by Dr. ___________.
PREOPERATIVE DIAGNOSIS:
Lumbosacral disk disease.
POSTOPERATIVE DIAGNOSIS:
Lumbosacral disk disease.
OPERATIVE PROCEDURE:
Anterior exposure for L4-L5 anterior lumbar interbody fusion with placement of cage and screws .
INDICATION:
This is a pleasant 60-year-old with severe lumbosacral disc disease and spondylolisthesis being scheduled for anterior lumbar interbody fusion, posterior instrumentation. The patient had a previous fusion at L5-Sl. She is now being taken to the operating room for her unstable L4-L5. The patient is aware of options and risks.
DESCRIPTION OF OPERATIVE PROCDURE
The patient was placed on her back on the operating table. General endotracheal anesthesia was administered without difficulty. Foley catheter and radial art line were placed. The abdomen was shaved, prepped and draped in the usual sterile fashion. After a brief preoperative time-out, the patient had an 8 em left paramedian incision made beginning just to the left of the umbilicus and extending down. It was carried down through subcutaneous tissue with Bovie electrocautery. The fascia was divided along the lines of skin incision. Medial aspect of the fascia was grasped with 2 Kelly clamps. The rectus was gently teased away from the posterior rectus sheath and retracted towards the left. Sponge s tick was used to help elevate the inferior epigastric artery and vein. The retroperitoneum was entered. A small portion of lateral flexion of posterior rectus sheath was divided with Bovie electrocautery and extended tip. Peritoneal contents were retracted towards the right. Psoas was visualized and genitofemoral nerve was avoided. Bookwalter retractor was set up with the post on the right using a small ring. Three blades were positioned. Dissection was carried out just to left of the left iliac artery. Bipolar electrocautery was necessary to divide some of the very small lymphatics to retract them to the left. Dissection was carried down on to a large segmental vein, right at the top of L4. This was ligated with 2-0 silk suture ligated with 5-0 Prolene, clipped and divided. The iliolumbar vein below the L4-L5 level was then identified. It was ligated with 2-0 s ilk suture ligated with 5-0 Prolene, clipped and divided. At that point, we just dissected the vessel off of the anterior surface of that ligament over L4-L5. There were several small venous perforators, which were coagulated with bipolar electrocautery and divided. The vein was mobilized without too much trouble and a bent spinal needle was then placed in the disk space. We confirmed that we are in the midline and at the appropriate level. I marked the midline with Bovie electrocautery and renewed the needle. At that point, Dr. _______ came into the room. He did his diskectomy at L4-L5 and placed a cage with 2 screws for fixation. A small amount of FloSeal was placed for complete hemostasis. The retractor blades were reviewed. Sponge, instrument and needle counts were correct. Final films were done, 4-quadrant films were done. The ureter, iliac artery and vein and inferior epigastric artery and vein were all seen to be without any injury. Pulse ox in left great toe read 1 000/o sat. The pulse in left foot was normal. SSEPs were baseline. The fascia of the rectus was closed with #1 Vicryl, one beginning superiorly and one inferiorly, tied in middle. Subcutaneous tissue was closed with two layers of 2-0 Vicryl and the skin with 3-0 Monocryl in a subcuticular fashion. Steri-Strips and dry sterile dressings were applied. The patient was then returned to the prone position for further instrumentation, dictated under separate cover by Dr. ___________.