I am in the mist of establishing an audit process for our practice. I have been in search of a valuable means of setting up a statistical audit system that could be performed on a quarterly basis. I am not looking computer program but rather a process that I can manually work. Has anyone out there established a statistical means of pulling a random sample and a concise way of reporting the results that is fairly user friendly?
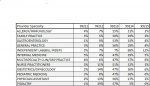
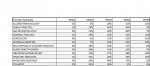
I compare my providers' E/M utilization to CMS's data, based on their provider type, and I select claims based on where they're outliers, like a RAC auditor would. You can find utilization stats here (2009 is the most recent data - they have a 2 year lag):
http://www.cms.gov/MedicareFeeforSvcPartsAB/04_MedicareUtilizationforPartB.asp
You have to go in and manually calculate the percentages (I already figured the percentages for a few common specialties for established E/M's 99211-99215...I attached a chart). So for example, if one of my Family Practice docs bills 75% of their visits as 99213's, and only bills 10% as 99214's, then I'll predominately pull 99213's, since they have the highest probability of being coded incorrectly. My goal is to identify high risk billing activities, so my audits are more targeted.
The other way to do it, is simply to add up all of the E/M's for a given time period, and pull a sample that's representive of what they bill. (More of a routine review, than a targeted review). So if 10% of their E/M's are 99212, 50% are 99213, 40% are 99214, and 10% are 99215, then you might pull 1 99212, 5 99213's, 4 99214's, and 1 99215 to review, at random. You don't really need software to do any of that, but it would be helpful to have an electronic database of the billing records for your location, so you can just run a report to find how many of each kind of E/M's you're sending out.
Also, when I perform a review, I try to only pull charts from a certain set of payers, so that the billing rules are uniform; usually, your safest bet is to go with only Medicare or Medicaid encounters, but I'll also pull claims from Blue Cross if I can't get enough govt. payer claims, since their rules are similar, and they have a 12 month filing deadline in my state (in the event that I find any corrections that need to be made).
Here's another really good resource:
http://www.ttuhsc.edu/billingcompliance/policies_procedures.aspx
Check out their policies and procedures for auditing their providers...they have a really great 'points' system that assigns values to mistakes, by how significant they are to the organization. The links you may find especially helpful include: "Coding and Documentation Improvement", "Annual Risk Assessment", "Routine Billing Compliance Monitoring", and for anyone who's on EMR/EHR, I highly recommend reading everything under "Chapters 7&8 - Electronic Health Records and Coding" - their policies are structured well enough that they could easily be adopted and changed to fit into a smaller practice's protocol, and I'm
fairly certain that they were developed as a result of some kind of action with the OIG a few years ago, so they should definitely be 'compliant' enough to keep your practice safe.
Hope that helps!