jessicamarquez05
Contributor
I just took over Rev Cycle for F&A and Wound offices, I don't have a ton of guidance.
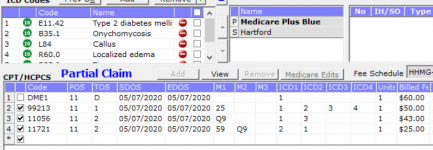
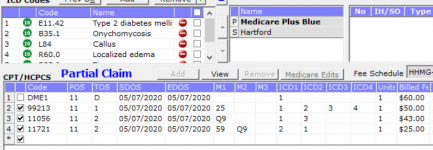
I have quite a few denials for Medicare Plus Blue and other BCBS products for codes 11056 and 11721.
My office does Medicare split billing, the UB usually pays but the HCFA portion denies. They are usually LCD Denials but from what I can tell these dx codes fit into the LCD. I am at a loss. I have to do CE appeals for almost all claims with these codes. The codes have the q9 modifier like they should and also the mod 59 to override bundling.
Here is an example:
anyone insight on this? Is anyone else having these issues?
Thanks,
Jessica
I have quite a few denials for Medicare Plus Blue and other BCBS products for codes 11056 and 11721.
My office does Medicare split billing, the UB usually pays but the HCFA portion denies. They are usually LCD Denials but from what I can tell these dx codes fit into the LCD. I am at a loss. I have to do CE appeals for almost all claims with these codes. The codes have the q9 modifier like they should and also the mod 59 to override bundling.
Here is an example:
anyone insight on this? Is anyone else having these issues?
Thanks,
Jessica