awolf214
New
Hello everyone,
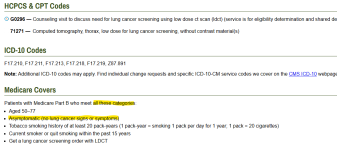
Looking for guidance for one of my coders. We are billing G0296 CT Low Dose Lung Counseling to Humana Choice Medicare. We attached Dx: Z87.891 to this code. Humana has denied this code stating payment is not allowed for this service because the diagnosis billed is not valid as a primary diagnosis. The supervisor coder states this should be a good dx code. I submitted a reconsideration that was denied for the same thing. I contacted Humana and they were no help ofcourse . They could not provide any policy nor Article on CMS Gov that would help. Looking for guidance from other coders.
. They could not provide any policy nor Article on CMS Gov that would help. Looking for guidance from other coders.
Other codes we are billing on this claim are: 99214, 96160, G0439, 99497, G0444, G0442, G0296
Dx's listed on claim but are not attached to G0296 are: R91.1, I10, E78.5, I25.10, K76.89, R73.9, C61, E66.9, Z00.00, Z13.31, Z13.39, Z78.9, J44.9
Modifiers attached to the claim : 25, 59, 33
I am not the coder on this claim just the Claims denial Representative.
I currently have my CPC-A but not currently in a coder job role.
Any help would be greatly appreciated.
Thank you
Looking for guidance for one of my coders. We are billing G0296 CT Low Dose Lung Counseling to Humana Choice Medicare. We attached Dx: Z87.891 to this code. Humana has denied this code stating payment is not allowed for this service because the diagnosis billed is not valid as a primary diagnosis. The supervisor coder states this should be a good dx code. I submitted a reconsideration that was denied for the same thing. I contacted Humana and they were no help ofcourse
Other codes we are billing on this claim are: 99214, 96160, G0439, 99497, G0444, G0442, G0296
Dx's listed on claim but are not attached to G0296 are: R91.1, I10, E78.5, I25.10, K76.89, R73.9, C61, E66.9, Z00.00, Z13.31, Z13.39, Z78.9, J44.9
Modifiers attached to the claim : 25, 59, 33
I am not the coder on this claim just the Claims denial Representative.
I currently have my CPC-A but not currently in a coder job role.
Any help would be greatly appreciated.
Thank you