andreareeder
Guest
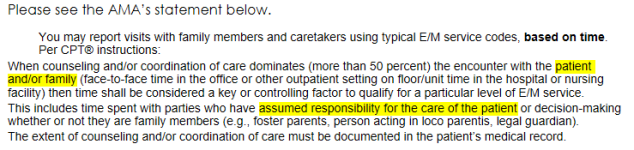
We have a number of providers asking if the patient must be present during a telehealth visit, and I am struggling to find a definitive answer.
One example would be a parent sets up a telehealth visit with pediatric specialist to ask questions regarding care of baby/child... does the baby/child have to be present on the call? What if the baby is napping, or the child is at school?
Another example would be adult children of an elderly patient. If there is a telehealth visit with the family caregiver, does the elderly patient need to be present on the visit?
I appreciate any feedback and reliable resources cited.
One example would be a parent sets up a telehealth visit with pediatric specialist to ask questions regarding care of baby/child... does the baby/child have to be present on the call? What if the baby is napping, or the child is at school?
Another example would be adult children of an elderly patient. If there is a telehealth visit with the family caregiver, does the elderly patient need to be present on the visit?
I appreciate any feedback and reliable resources cited.