They are looking for information on whether the entire vial was administered or if there was drug waste. If the entire vial was administered, then you would bill
JZ-Zero drug amount discarded/not administered to any patient. If the entire vial was not administered, then you need to bill 2 lines for this code with one line for the units administered without a modifier and then bill a second line for the code with the number of units wasted/discarded and append modifier
JW-Drug amount discarded/not administered to any patient.
For example, which is based on fictitious information for the units on this J code:
- if the vial contained 100 units and the patient was administered all 100 units you would bill J7327-JZ 100 units.
- if the vial contained 100 units and the patient was administered 75 units you would bill 1 line as J7327 75 units and the second line you would bill J7327-JW 25 units.
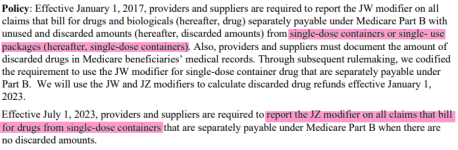
Effective 07/01/23 for single dose vials were there was no drug waste modifier JZ is required to be billed with the J code to indicate that the patient received the entire contents of the vial, the modifier was effective 01/01/23 and it was optional to use 01/01/23-06/30/23 but as of 7/1/23 it is mandatory.
You can review IOM 100-04
Claims Processing Manual: Chapter 17-Drugs and Biologicals; section 40-40.1 as well as this FAQ regarding
Discarded Drugs and Biologicals – JW Modifier and JZ Modifier Policy Frequently Asked Questions
Hopefully these resources will help you get your claims submitted and processed correctly.