jamiepeters
Networker
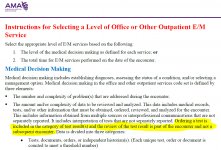
If a provider orders a test such as MRI (that we are not billing for) is it included In the MDM at this time? If it is included in MDM when ordered can you also include it in MDM when the patient returns for review of the results in a subsequent encounter?
Email response regarding the same question. I am finding other info through my own research so I am not sure what is correct and wanted to find out what everyone else is doing in this situation.
The category for data per the AMA is based on date of service, when leveling the E/M. So my understanding is as follows: Date of Service a: order was made (yes it can be counted). if results will take of couple of days patient returns Date of Service b to discuss those results and further treatment protocol, then yes it can be counted again. It remains a date of service element; point of care.
Email response regarding the same question. I am finding other info through my own research so I am not sure what is correct and wanted to find out what everyone else is doing in this situation.
The category for data per the AMA is based on date of service, when leveling the E/M. So my understanding is as follows: Date of Service a: order was made (yes it can be counted). if results will take of couple of days patient returns Date of Service b to discuss those results and further treatment protocol, then yes it can be counted again. It remains a date of service element; point of care.
Last edited: