TrinaJKGarcia
Guest
- Messages
- 3
- Best answers
- 0
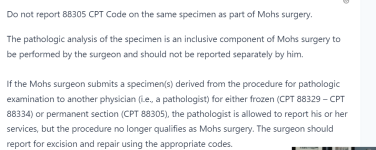
We are a dermatology office whose doctor is a certified dermatopathologist as well. He can perform MOHS. We have come across a new issue with Medicare when billing MOHS and a separate pathology on the same day. Here is an example: Patient comes in and has MOHS done on the arm by the doctor. The patient also has a separate excision performed on the face by one of our ARNP's, that excision requires a pathology to be billed. So we bill for the MOHS, the MOHS closure, then the excision and closure of the other lesion and the pathology--that is done by the Dr who performed the MOHS. We have in the past been able to add a 59 modifier to the 88305 indicating that it is separate than the MOHS, but now Medicare is denying the 88305 still. Anyone encounter this, or have any information?