xXxPARAGONxXx
Guest
The following is a practice test question that I took recently:
MEDICAL RECORD
SEX: MALE
AGE: 47
DOS: 1/1/20XX
PHYSICIAN:
PREOPERATIVE DIAGNOSIS: Family history of colon cancer and multiple colon polyps.
POSTOPERATIVE DIAGNOSIS: Normal colon.
OPERATIVE PROCEDURE: Screening Colonoscopy with Conscious Sedation. Time 19 min.
SURGEON:
FINDINGS: The patient is a male with regular bowel movements and no history of bleeding, and whose family, multiple people, who has had multiple colon polyps and colon cancer. His examination shows essentially normal rectum. His prostate does not feel enlarged, but is difficult to palpate because of his body habitus. The remainder of his colon is well prepared and the mucosa appears normal, without evidence of pathology. I would recommend maintaining adequate fiber intake in his diet and repeat colonoscopy at age 50, or sooner if he develops bowel habit change or bleeding.
TECHNIQUE: After explaining the operative procedure, the risks, and potential complications of bleeding and perforation, the patient was given 320 mg of propofol intravenously for conscious sedation by me. His pulse was 70, saturations 97, blood pressure 134/83. A rectal examination was done and then the colonoscope was inserted through the anorectum, rectosigmoid, descending, transverse, and ascending colon to the ileocecal valve. The areas were examined carefully. Then, the air and instrument were gradually withdrawn. The patient tolerated the procedure well.
Analgesia/sedation given. Patient status during sedation was attended constantly and was cooperative. Vitals were stable monitored.
Electronically signed by 1/1/20XX
I have to provide the correct Primary Diagnosis, Secondary Diagnosis, and CPT after reviewing the Medical Record (above). Here are the answers I submitted:
My question concerns the CPT answer I submitted, 45378 Unit 1 Mod 33, versus the "correct" answer, 45378 Unit 1.
I reported the "correct" answer to be reviewed by the staff. The test I am taking has quite a few erroneous "correct" answers, so it is common for me to report answers. Often they explain how I am wrong, and I recognize my error. Other times they recognize that the test answer is wrong, and they submit a report on their end to correct it.
This is what I typed into my Report Request:
Per 2024 CPT,
(This is a non-Medicare patient.) My understanding is that for a screening colonoscopy, I would append modifier -33 to 45378 to inform the payer that 45378, which by description is a diagnostic colonoscopy, is being performed as a screening colonoscopy. This is to ensure that the payer does not require the patient to pay a co-pay, etc.
The person who reviewed my report replied as follows,
I do not believe the person is correct. I believe my usage of modifier 33 is correct and in agreement with the references I cited.
Pleas let me know if my assertion is incorrect.
MEDICAL RECORD
SEX: MALE
AGE: 47
DOS: 1/1/20XX
PHYSICIAN:
PREOPERATIVE DIAGNOSIS: Family history of colon cancer and multiple colon polyps.
POSTOPERATIVE DIAGNOSIS: Normal colon.
OPERATIVE PROCEDURE: Screening Colonoscopy with Conscious Sedation. Time 19 min.
SURGEON:
FINDINGS: The patient is a male with regular bowel movements and no history of bleeding, and whose family, multiple people, who has had multiple colon polyps and colon cancer. His examination shows essentially normal rectum. His prostate does not feel enlarged, but is difficult to palpate because of his body habitus. The remainder of his colon is well prepared and the mucosa appears normal, without evidence of pathology. I would recommend maintaining adequate fiber intake in his diet and repeat colonoscopy at age 50, or sooner if he develops bowel habit change or bleeding.
TECHNIQUE: After explaining the operative procedure, the risks, and potential complications of bleeding and perforation, the patient was given 320 mg of propofol intravenously for conscious sedation by me. His pulse was 70, saturations 97, blood pressure 134/83. A rectal examination was done and then the colonoscope was inserted through the anorectum, rectosigmoid, descending, transverse, and ascending colon to the ileocecal valve. The areas were examined carefully. Then, the air and instrument were gradually withdrawn. The patient tolerated the procedure well.
Analgesia/sedation given. Patient status during sedation was attended constantly and was cooperative. Vitals were stable monitored.
Electronically signed by 1/1/20XX
I have to provide the correct Primary Diagnosis, Secondary Diagnosis, and CPT after reviewing the Medical Record (above). Here are the answers I submitted:
| My Answer | Correct Answer | |
| Primary Diagnosis | Z12.11 | Z12.11 |
| Secondary Diagnosis | Z83.71 | Z83.71 |
| Z80.9 | Z80.0 | |
| CPT | 45378 Unit 1 Mod 33 | 45378 Unit 1 |
| 99152 Unit 1 | 99152 Unit 1 |
My question concerns the CPT answer I submitted, 45378 Unit 1 Mod 33, versus the "correct" answer, 45378 Unit 1.
I reported the "correct" answer to be reviewed by the staff. The test I am taking has quite a few erroneous "correct" answers, so it is common for me to report answers. Often they explain how I am wrong, and I recognize my error. Other times they recognize that the test answer is wrong, and they submit a report on their end to correct it.
This is what I typed into my Report Request:
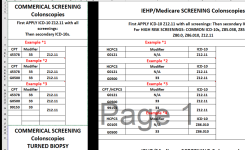
PER CPT 2024, P. 971, "33 - PREVENTIVE SERVICES: WHEN THE PRIMARY PURPOSE OF THE SERVICE IS THE DELIVERY OF AN EVIDENCE BASED SERVICE IN ACCORDANCE WITH A US PREVENTIVE SERVICES TASK FORCE A OR B RATING IN EFFECT AND OTHER PREVENTIVE SERVICES IDENTIFIED IN PREVENTIVE SERVICES MANDATES (LEGISLATIVE OR REGULATORY), THE SERVICE MAY BE IDENTIFIED BY ADDING 33 TO THE PROCEDURE. FOR SEPARATELY REPORTED SERVICES SPECIFICALLY IDENTIFIED AS PREVENTIVE, THE MODIFIER SHOULD NOT BE USED." ALSO, SEE HTTPS://www.aafp.org/PUBS/FPM/ISSUES/2016/0700/P38.HTML. "MODIFIER 33 WAS ADDED IN RESPONSE TO THE PATIENT PROTECTION AND AFFORDABLE CARE ACT PROVISION THAT REQUIRES INSURERS TO COVER CERTAIN PREVENTIVE SERVICES AND IMMUNIZATIONS WITHOUT COST SHARING TO THE PATIENT. WHEN BILLING FOR SERVICES THAT COULD BE EITHER PREVENTIVE OR DIAGNOSTIC (E.G., 45378, COLONOSCOPY), USE MODIFIER 33 TO INDICATE THAT THE CODE REPRESENTS A COVERED PREVENTIVE SERVICE. THIS ENSURES THAT THE PATIENT WILL NOT BE SUBJECT TO A COPAYMENT OR DEDUCTIBLE. HOWEVER, IF A SERVICE IS ALREADY IDENTIFIED AS PREVENTIVE WITHIN THE DEFINITION, DO NOT USE MODIFIER 33 (E.G., 77057, SCREENING MAMMOGRAPHY, BILATERAL)."
Per 2024 CPT,
45378 Colonoscopy, flexible; diagnostic, including collection of specimen(s) by brushing or washing, when performed (separate procedure)
(This is a non-Medicare patient.) My understanding is that for a screening colonoscopy, I would append modifier -33 to 45378 to inform the payer that 45378, which by description is a diagnostic colonoscopy, is being performed as a screening colonoscopy. This is to ensure that the payer does not require the patient to pay a co-pay, etc.
The person who reviewed my report replied as follows,
Modifier 33 does not apply as no additional procedure was performed such as a biopsy (45380). Modifier 33 is appended when a screening colonoscopy converts to a therapeutic (such as a biopsy or polypectomy).
I do not believe the person is correct. I believe my usage of modifier 33 is correct and in agreement with the references I cited.
Pleas let me know if my assertion is incorrect.