MarilynS
Networker
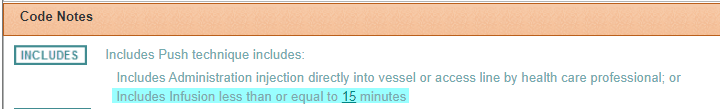
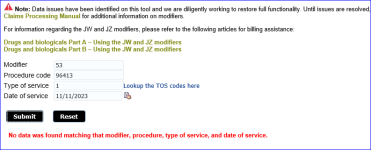
Patient comes in for an infusion of Actemra. Patient starts not to feel good. Doctor ends the infusion before its complete. I billed 96413 and J3262 with mod 53. Humana denied saying modifier is inconsistent with procedure code or required modifier is missing. So I sent a corrected claim adding modifier JZ. Humana denied claim again with same denial verbiage. I'm at a loss. I don't know what they want. Please help. Thanks!!