Dr. Pechacek, we are being told by our medical providers that a pressure ulcer will always be reported at it's initial severity for the duration of the wound, even if consistent care is being performed and wound is healing to a lesser stage. We believe per coding guidelines that the wound staging should be updated according to its current stage at the time of the encounter.
EX 01/01/20xx Pt presents with stage 4 sacral pressure ulcer
After continuous treatment, on 03/01/20xx wound now presents as a stage 2 sacral pressure ulcer.
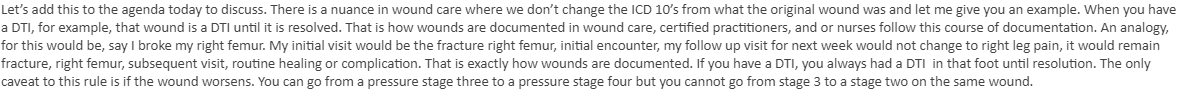
Providers believe that as of 03/01/20xx they should still code it as stage 4, that the wound will always be a stage 4 ulcer until it fully heals, or worsens.
we as coders believe that at this point in time, for DOS 03/01/20xx it should be coded as stage 2.
What are your thoughts on this scenario? Any guidance on how we can bridge this knowledge gap with our providers and overcome the pushback that we get on this subject? Unless we are in the wrong, I would love to understand more.
Please see attached the guidelines we have found and the email response from our provider.
Thanks a million!