dhunterc
New
Hi all!
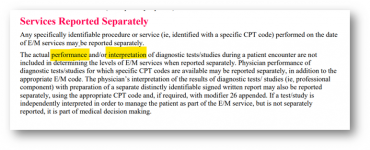
I know this question keeps circulating but I only see where people comment that they heard or that someone told them that if you bill for a test that you cannot count the order as part of MDM. Can someone please point me to specific written guidance on this? AMA says the actual performance or interpretation of the test cannot be included if you are billing separately - which makes sense. But where is the credit for the MDM to actually order the test? If we don't bill the test in house, we get the MDM credit for ordering it, why should it be any different if we bill for it? The CPT for the test does not include any E/M component - what about the work it takes for the provider to decide which test should be order for the patient - should that not be given credit as part of MDM?
TIA!!
I know this question keeps circulating but I only see where people comment that they heard or that someone told them that if you bill for a test that you cannot count the order as part of MDM. Can someone please point me to specific written guidance on this? AMA says the actual performance or interpretation of the test cannot be included if you are billing separately - which makes sense. But where is the credit for the MDM to actually order the test? If we don't bill the test in house, we get the MDM credit for ordering it, why should it be any different if we bill for it? The CPT for the test does not include any E/M component - what about the work it takes for the provider to decide which test should be order for the patient - should that not be given credit as part of MDM?
TIA!!