lisaray
New
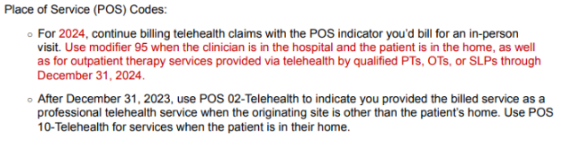
I am very confused why all of a sudden we are seeing denials using place of service 11 with modifier 95 and now they want us to use POS 10 for telehealth in patient's home and POS 02 if they are not home. It seems to vary by payer and I know some are following Medicare guidelines but we are being reimbursed less using this place of service. It takes just as much time and effort to conduct services. Why do they pay less? I just received a denial on a claim for a Humana Medicare advantage claim. Anyone have any input or knowledge would be much appreciated. I did see there is a bulletin on Humana's website via availity noting a change. Here is how claim processed
Procedure DOS Code Type Code TranslationHC: 99213:95 01/03/2024 HE M77 Missing/incomplete/invalid/inappropriate place of service.
We used POS 11 Anyone else seeing this issue? Thanks
Procedure DOS Code Type Code TranslationHC: 99213:95 01/03/2024 HE M77 Missing/incomplete/invalid/inappropriate place of service.
We used POS 11 Anyone else seeing this issue? Thanks