ejthornton
Contributor
We have a provider that does time based coding, but they are only spending 7 or 9 mins with the patient, can I bill a 99212?
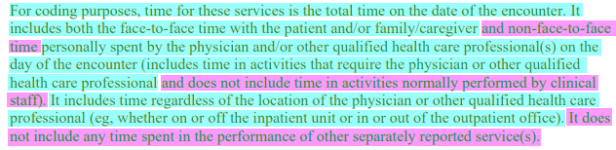
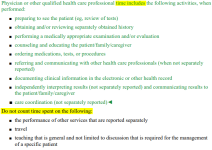
Hi there, you cannot. As noted above you should remind the provider that they can count non-face-to-face time on the date of the encounter. If a QHP also contributes to the encounter, you can combine their time.We have a provider that does time based coding, but they are only spending 7 or 9 mins with the patient, can I bill a 99212?
This is why I discourage clients I work with from coding based upon time. In many cases, the visits would be under coded if chosen based upon time.Can you clarify what you mean when you stated, "the documentation in the note shows a level 4.", is this information entered by the provider's documentation of the visit? The minimum time required for a level 4 visit is 30 minutes. Is there any chance that the visit was documented as a level 4 based on MDM and not time? If so, when you review the record does the claim meet the MDM criteria for a level 4 visit?
If the claim wasn't leveled based on MDM and time is being used, then no, a 15-minute visit doesn't meet the minimum time requirement for a level 4 visit which is at least 30 minutes. If the E&M is being leveled on time alone based on the time documented being 15-minutes, this would be a 2 which is a minimum of 10 minutes and unfortunately the minimum time for a level 3 visit is a minimum of 20 minutes.
When you say, "does time based coding", do you mean they document the time in every visit note and expect that the visit will be coded by time for each one? Is the EMR just a template that is automatically filling that field out but the provider doesn't actually "choose" it? How do you know they are spending 7-9 minutes, does it say that in the documentation? What does the full documentation actually say?We have a provider that does time based coding, but they are only spending 7 or 9 mins with the patient, can I bill a 99212?