- Messages
- 30
- Best answers
- 0
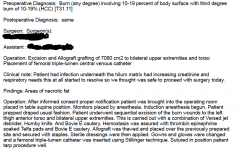
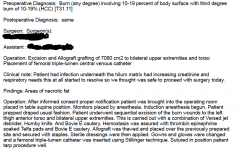
We've been getting pushback from UHC and Optum on our op notes. They are stating they cannot verify the surgeries we are billing were documented. I have screen shot a sample of a note below. There's the pre/post op diagnosis and the operation synopsis listed of the exact graft we billed. They are stating since the type of graft and sq cm are not repeated within the operation body, they won't pay the claim. Does anyone have a resource or a reference that would allow me to dispute this?
In the meantime, I have having the physicians repeat the information in the body, but I don't believe there is a requirement on this particular issue.
In the meantime, I have having the physicians repeat the information in the body, but I don't believe there is a requirement on this particular issue.