Tiffanynora
New
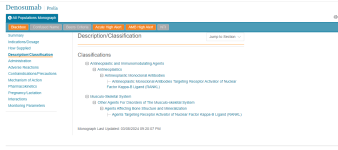
Question about diagnosis for patients that are seen in infusion clinics for the "Prolia (denosumab)" injection.
I am being instructed to code Z51.15 - Encounter for antineoplastic immunotherapy as the Primary Diagnosis following the providers diagnosis (M81.0) for these encounters for when the patient is seen for their injection.
Should I be including the "Z51.12" DX code?
I am not finding any information to support billing this way.
My sources of information: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=52399&ver=50&=
https://www.proliahcp.com/-/media/T...162_82995_Prolia-Billing-and-Coding-Guide.pdf
I am being instructed to code Z51.15 - Encounter for antineoplastic immunotherapy as the Primary Diagnosis following the providers diagnosis (M81.0) for these encounters for when the patient is seen for their injection.
Should I be including the "Z51.12" DX code?
I am not finding any information to support billing this way.
My sources of information: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=52399&ver=50&=
https://www.proliahcp.com/-/media/T...162_82995_Prolia-Billing-and-Coding-Guide.pdf