Korbc
Expert
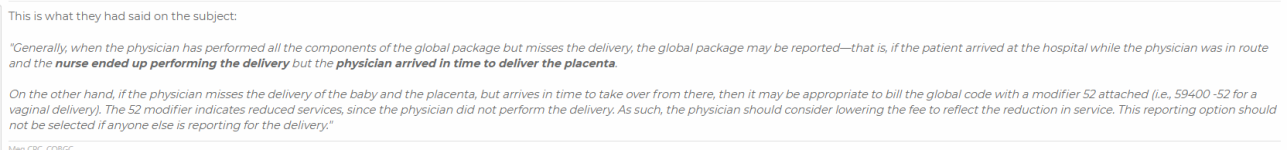
In this newsletter they mention if a nurse delivers because the doctor in busy in the next room per say doing something if other people have been using 52 on their global deliveries? and then quote "Be sure to include information about which part of the process they did participate in, so you’ll lessen the impact of any fee reduction the payer might apply." Does that mean to send in our notes to the insurer pointing out what our midwife did? Should I even use 52 if your midwives delivered?
Also another question, I did see this article quote "The delivery-only CPT® code does not include rounding visits in the hospital, nor discharge, which would be coded separately per CPT® instructions"
I don't really see any specific guidelines on how to bill for this, ....... would you code rounding visits as subsequent hosp. care or code the first rounding visit as initial hosp care and then the others as subsequent, and then a discharge day management hosp. code on the day they discharge? And if they deliver and discharge on the same day, even though I don't think I've encountered that yet would you use 99234-99236 with the delivery only code?
Thanks so much!
Also another question, I did see this article quote "The delivery-only CPT® code does not include rounding visits in the hospital, nor discharge, which would be coded separately per CPT® instructions"
I don't really see any specific guidelines on how to bill for this, ....... would you code rounding visits as subsequent hosp. care or code the first rounding visit as initial hosp care and then the others as subsequent, and then a discharge day management hosp. code on the day they discharge? And if they deliver and discharge on the same day, even though I don't think I've encountered that yet would you use 99234-99236 with the delivery only code?
Thanks so much!