CatchTheWind
Guest
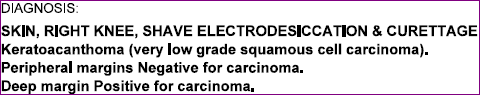
To those of you who are familiar with the problem surrounding the coding of keratoacanthoma (whereby dermatologists consider it to be a form of squamous cell carcinoma, whereas ICD-10 codes it as "L85.8" (other specified dermal thickening)):
Is it possible to code a malignant excision with L85.8 as the diagnosis? Alternately, is there any source that justifies coding the keratoacanthoma as an SCC, in spite of the fact that ICD-10 states otherwise?
Is it possible to code a malignant excision with L85.8 as the diagnosis? Alternately, is there any source that justifies coding the keratoacanthoma as an SCC, in spite of the fact that ICD-10 states otherwise?