SarahSee1114
Networker
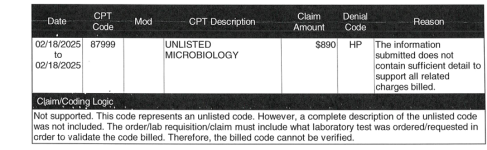
I'm struggling trying to learn lab coding. I haven't found anyplace to learn, no AAPC resources or local chapter help has been available so I'm trying to educate myself. Everything I've seen states to just match up the test to the code, which doesn't seem to be very real world situation. I'm working appeals so I'm seeing documentation and claims on the back end.
Please help me understand how the following list of respiratory labs are coded by 4 codes. I understand 87633 is for 12-25 targets, but I don't know which ones. And I also found that these tests were performed by QiStat Respiratory SARS-CoV2 panel and should be billed by 0223U. Is it subjective whether four CPT codes are billed vs. the PLA lab code? Any help at all is appreciated!
Codes: 87486, 87581, 87633, 87798
Adenovirus DNA
Coronavirus_229E (not Covid 19)
Coronavirus_NL63
Coronavirus_HKU1
Coronavirus_OC43
Human Metapneumovirus
Human Rhinovirus/Enterovirus
Influenza A H3
Influenza A H1
Influenza A H1N1/pdm09
Parainfluenza 1
Parainfluenza 2
Influenza A
Influenza B
Parainfluenza 3
Parainfluenza 4
Respiratory Syncytial Virus
Bordetella Pertussis
Chlamydophila pneumoniae - 87486
Mycoplasma pneumoniae - 87581
Covid 19(SARS-CoV2-2)
Please help me understand how the following list of respiratory labs are coded by 4 codes. I understand 87633 is for 12-25 targets, but I don't know which ones. And I also found that these tests were performed by QiStat Respiratory SARS-CoV2 panel and should be billed by 0223U. Is it subjective whether four CPT codes are billed vs. the PLA lab code? Any help at all is appreciated!
Codes: 87486, 87581, 87633, 87798
Adenovirus DNA
Coronavirus_229E (not Covid 19)
Coronavirus_NL63
Coronavirus_HKU1
Coronavirus_OC43
Human Metapneumovirus
Human Rhinovirus/Enterovirus
Influenza A H3
Influenza A H1
Influenza A H1N1/pdm09
Parainfluenza 1
Parainfluenza 2
Influenza A
Influenza B
Parainfluenza 3
Parainfluenza 4
Respiratory Syncytial Virus
Bordetella Pertussis
Chlamydophila pneumoniae - 87486
Mycoplasma pneumoniae - 87581
Covid 19(SARS-CoV2-2)