lcouto
Networker
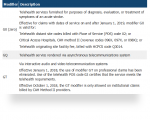
Thank you for clarifying and for your time.. I appreciate itFrom my understanding, 99212-99215 are used ONLY for telehealth which is interactive audio and video (note that they have temporarily lifted many requirements, and the interactive audio/video may be via Skype, FaceTime, etc.)
99421-99423 are for patient portal.
99441-99443 are for telephone.
MEDICARE TELEMEDICINE HEALTH CARE PROVIDER FACT SHEET | CMS
Medicare coverage and payment of virtual services INTRODUCTION:www.cms.gov
EVERYONE WITH ADDITIONAL QUESTIONS SHOULD FIRST READ THIS ENTIRE THREAD. I'm seeing a lot of duplicate postings and questions