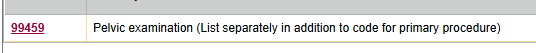
There may not be a workaround. This was a post from me a few weeks ago on a very similar thread about 99459:
I did some brief investigation tonight and we are also seeing denials with specific insurances when billing preventive with 99459. Most of the denials are diagnosis related (CO11, MA63, M76). Our organization is appealing these.
I'll note there are several possibilities.
1) Because it is coded appropriately does not mean the carrier will pay for it. Many payors have bundling rules over and above NCCI edits. The carrier may never pay for 99459 with a preventive diagnosis.
2) The carrier did not intend to deny, but did not properly load 99459 into their claims processing system.
3) The carrier wants to review these individually (kind of like when some carriers flag modifier -25) and determine whether or not to pay.
4) Any and all of the above, plus any other reason a payor will decide to not pay a claim.
PS - I have also seen some carriers bundle 99459 with E&M 99202-99215, but not many. In fact, one paid the 99459 and denied 99214.

Those are also being appealed.