I have been having a discussion with my OBGyn providers about the documentation required for Assistant at surgery (Modifier 80). I have been telling them, based on what I have found and read in various articles, that they need to include documentation of why an assistant was needed and what the assistant did during the operative session. I have provided them the resources that I have found that are stating this documentation is required, but they are still fighting me on it. I am at a loss of what else to tell them to support that they need to provide this documentation. Maybe if I could show them where CMS says it? I have looked on CMS and can't find any documentation to support this and I have seen several questions on AAPC from people asking where in CMS it states this documentation is required. Any help that anyone could provide on this subject would be greatly appreciated! Thanks
-
If this is your first visit, be sure to check out the FAQ & read the forum rules. To view all forums, post or create a new thread, you must be an AAPC Member. If you are a member and have already registered for member area and forum access, you can log in by clicking here. If you've forgotten your username or password use our password reminder tool. To start viewing messages, select the forum that you want to visit from the selection below..
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Wiki Assistant at Surgery
- Thread starter CFINDLING
- Start date
Hi, I don't know that it is a CMS requirement - it may be - but it's also very much a reimbursement issue. Many payers will not reimburse an assistant without this information.
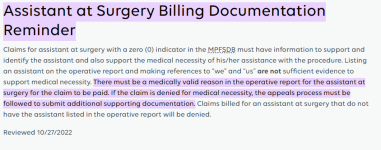
Here's a link to the Novitas assistant at surgery modifier fact sheet - there are links there to CMS where you might find what you're looking for, but it does state "The operative note should clearly document the assistant surgeon's role during the operative session." You can also check your specific state's contractor. https://www.novitas-solutions.com/webcenter/portal/MedicareJL/pagebyid?contentId=00144529
Also NGS https://www.ngsmedicare.com/web/ngs...to submit additional supporting documentation.
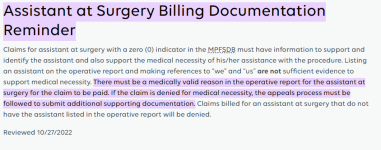
Here's a link to the Novitas assistant at surgery modifier fact sheet - there are links there to CMS where you might find what you're looking for, but it does state "The operative note should clearly document the assistant surgeon's role during the operative session." You can also check your specific state's contractor. https://www.novitas-solutions.com/webcenter/portal/MedicareJL/pagebyid?contentId=00144529
Also NGS https://www.ngsmedicare.com/web/ngs...to submit additional supporting documentation.
Last edited:
amyjph
True Blue
Show them in $$ - denials and take backs from operative report submission where the payer either denies a claim for the assistant, or takes back payment later when they audit it.
Just because the CPT "always" allows an assistant doesn't mean it will be paid/covered just because their name is on the report. If there is no indication of what they did or why they were needed it probably would not be paid if the payer looks at the op report. Look to the words, "actively assists". How do you know what they were doing if only their name is listed at the top and nothing else?
These are examples, you would have to look up for your state/payer:
Here is on MAC example where it says it: https://www.novitas-solutions.com/webcenter/portal/MedicareJL/pagebyid?contentId=00144529
The "assistant at surgery" provides more than just ancillary services. The operative note should clearly document the assistant surgeon's role during the operative session.
Payer example: https://www.bluecrossmn.com/sites/d...ional-procedure-001-assistant-at- surgery.pdf
Documentation Submission The documentation/operative report should include the name and credentials of the assistant, and the specific activities that the assistant at surgery performed.
An Assistant-at-Surgery actively assists the Physician performing a surgical procedure.
An assistant at surgery is a provider who actively assists the physician in charge of a case in performing a surgical procedure.
Other discussions:
"To bill for an assistant at surgery, the surgeon is required to specify in the body of the operative report what the assistant actually does. It is not sufficient evidence of participation to list the assistant’s name in the heading of the operative report. It is also a good idea to mention in the indications paragraph why there is a need for an assistant. Carriers that request the op report in order to process the assistant’s claim will deny claims if there is no accounting by the surgeon for what was performed by the assistant."
"Operative notes should highlight assistant surgeon’s role
The body of the operative note needs to include what the assistant surgeon contributed to the surgery and their role in the session. Also ensure that the name and credentials of the assistant surgeon are documented. To support modifier 82, the operative note should also state why there was no qualified resident available and why a non-resident assistant had to assist with the surgery."
Just because the CPT "always" allows an assistant doesn't mean it will be paid/covered just because their name is on the report. If there is no indication of what they did or why they were needed it probably would not be paid if the payer looks at the op report. Look to the words, "actively assists". How do you know what they were doing if only their name is listed at the top and nothing else?
These are examples, you would have to look up for your state/payer:
Here is on MAC example where it says it: https://www.novitas-solutions.com/webcenter/portal/MedicareJL/pagebyid?contentId=00144529
The "assistant at surgery" provides more than just ancillary services. The operative note should clearly document the assistant surgeon's role during the operative session.
Payer example: https://www.bluecrossmn.com/sites/d...ional-procedure-001-assistant-at- surgery.pdf
Documentation Submission The documentation/operative report should include the name and credentials of the assistant, and the specific activities that the assistant at surgery performed.
An Assistant-at-Surgery actively assists the Physician performing a surgical procedure.
An assistant at surgery is a provider who actively assists the physician in charge of a case in performing a surgical procedure.
Other discussions:
"To bill for an assistant at surgery, the surgeon is required to specify in the body of the operative report what the assistant actually does. It is not sufficient evidence of participation to list the assistant’s name in the heading of the operative report. It is also a good idea to mention in the indications paragraph why there is a need for an assistant. Carriers that request the op report in order to process the assistant’s claim will deny claims if there is no accounting by the surgeon for what was performed by the assistant."
"Operative notes should highlight assistant surgeon’s role
The body of the operative note needs to include what the assistant surgeon contributed to the surgery and their role in the session. Also ensure that the name and credentials of the assistant surgeon are documented. To support modifier 82, the operative note should also state why there was no qualified resident available and why a non-resident assistant had to assist with the surgery."
nielynco
True Blue
You might also want to access the College of Surgeons document "Assistants at Surgery" which lists all the procedure codes and indicates whether an assistant is sometimes, never or always needed during a particular surgery. This document is used by many payers and if you should get a denial but this document indicates one is almost always needed you may be able to win the appeal. The 2023 update to this document can be found at: https://www.facs.org/media/gp3ny4ps/2023-update-physicians-as-assistants-at-surgery.pdf